
UPDATED - originally published on October 3, 2017
Throughout UC, resourceful faculty and students who are committed to improving world health are turning out technologies to help governments, surveillance workers and doctors detect and treat diseases that are all too prevalent in poor countries.
A wealth of knowledge and data come from basic science laboratories, computer centers where millions of data are mined and sorted, gritty groundwork and even outer space.
UC effort and research result in valuable, handy and low-cost tools to help cash-strapped regions battle a variety of infectious diseases.
Shutting down malaria
Malaria is one of the deadliest diseases on Earth. But, remarkable progress has been made over the past 50 years and now several countries are on the verge of eliminating this mosquito born disease.
DiSARM (Disease Surveillance and Risk Monitoring) – developed and refined continuously by UCSF researchers – could be the technological closer to make eliminating countries finally malaria-free.
In malaria-eliminating countries, health workers in remote villages typically go house to house to track every case of malaria and collect a GPS point with the precise infection locations. DiSARM combines that data with satellite imagery – collected and sorted by scientists using Google Earth Engine – of conditions such as rainfall, temperature, vegetation, water proximity and elevation, all of which affect mosquito breeding and parasite growth.
“It produces ‘risk maps’ for health programs which must decide how best to use scarce resources immediately and in the future,” explained Hugh Sturrock, PhD, assistant professor of epidemiology and biostatistics, who leads the DiSARM project for the UCSF Global Health Group’s Malaria Elimination Initiative.
DiSARM provides malaria programs a near real-time view of the disease and where – even in the tiniest geographic pockets -- it could strike. Using machine learning, DiSARM can also predict which buildings are residential, and require visiting, and which are commercial or other non-residential. Combined with risk maps, programs can then plan where to deliver interventions such as insecticide spraying, mosquito nets or antimalarial treatments down to specific individual households.
These highly precise risk maps are critical in malaria-eliminating countries, as they get close to zero cases. “Often, countries make the mistake of cutting their efforts too soon,” he said. “Malaria can rebound quickly. But with these maps, health workers will be alerted and know when and where to target their resources until the disease is totally eliminated.”
If a malaria case is pinpointed in a low and wet area, for example, the map can steer surveillance workers to other areas with similar geographic and environmental conditions.
DiSARM is also accessible on mobile devices so that field teams can see locations of buildings they need to target using offline maps. They also can use the app to collect data even when they don’t have connectivity in remote areas, said Sturrock
DiSARM is being implemented in Namibia, Botswana, Zimbabwe and Swaziland with support from the Clinton Health Initiative, whose staff helps to provide constant feedback about the crucial data they collect in villages, schools, hospitals and other locations that are rigorously monitored.
For example, in Zimbabwe, which has achieved a sharp decline in malaria – a 74 percent drop in cases from 2005 to 2015 – DiSARM supports indoor residual spraying efforts in two provinces – Matabeleland South and North – that are on the cusp of malaria elimination.
But DiSARM is not only a valuable closer. Malaria afflicts 212 million people worldwide and kills some 429,000, mostly children, and the tool has great potential in the global fight against the disease. “Even in higher transmission settings, there is a need to ensure places are sprayed and to monitor progress, which DiSARM is designed to do,” said Sturrock.
And while the technology was developed to target malaria, DiSARM is flexible and can be adapted to predict other infectious and mosquito-borne diseases such as Zika, Dengue and Chikugunya.
In addition to risk mapping, it has potential for treatment and disease control, even in urban areas of high-risk countries, said Sturrock. In Swaziland, Zimbabwe and Botswana, millions of buildings are being mapped. Again, by combining surveillance and satellite data, health workers, for example, can identify and target building specific residents for vaccination or prevention programs.
The beauty of DiSARM is that it gives the power of prediction to intervention teams on the ground through a single platform that analyzes the many factors that contribute to a disease.
Low-cost tool checks HIV levels
They were once rivals – two teams of brilliant UC San Diego students, each with a noble cause. They competed against each other for three years in several contests, including the global health track at Big Ideas@Berkeley contest and the Social Innovation Challenge at the University of San Diego. They alternated first and second place finishes.
Finally, they heeded some other smart person’s advice: “If you can’t (always) beat em, join em.” And poor countries dealing with the HIV epidemic could end of benefiting.
Six of the students formed a company, Worldcare Technologies to develop a low-cost device to monitor the amount of HIV in the bloodstream.
People with HIV in countries like the U.S. who have access to standard therapy have their viral load tested regularly to make sure their treatment is working. Thus, doctors can alter therapy if, for example, the virus becomes resistant to prescribed drugs.
In poor countries hit hard by HIV, however, equipment and money are not available for regular measuring of HIV, and that deters optimal treatment, explained Kirk Hutchison, a senior at UC San Diego and CEO of Worldcare.
In July, Worldcare took first place at the National Academy of Engineering 2017 Global Grand Challenges Summit, and the company will use the $25,000 prize money to build out its prototype viral load testing system and to eventually manufacture the product on a large scale.
Its technology involves three steps: extracting RNA from a blood sample, amplifying a gene specific to HIV via polymerase chain reaction (PCR), and imaging on a microchip. It gives doctors a picture of viral load. If therapy is working, viral load remains low. But if levels are high, it’s a sign that the virus has become resistant and medication may need to change.
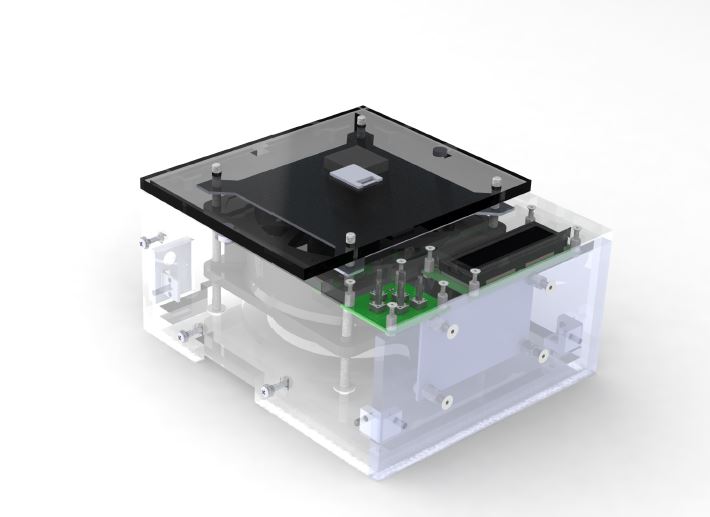
The process isn’t novel, but the real aim is an inexpensive test, said Hutchison. Currently, viral load test equipment costs around $80,000 and $25 or more per test. Worldcare’s award-winning prototype costs under $1,000, and it is easy to use, maintain and repair. Its projected cost per test is $8, but with refinements, Hutchison believes they can get the test cost to under $1.
They have enlisted the help of UC San Diego HIV and engineering researchers to improve the technology. Eventually – perhaps by next year – they hope to conduct clinical trials of the device in Tijuana, Mexico, close to their campus.
“It’s empowering to realize that even as students, it is possible to make a difference in the world,” said Hutchison.
Worldcare is advised by Davey Smith, MD, MAS, is professor of meedicine in the Division of Infectious Diseases and co-director of the UC San Diego Center for AIDS Research. It is made of members of two student groups:
- The Global TIES Open Viral Load team which is “working to build an affordable, open source viral load testing system for use in the developing world.” It is part of the larger Global TIES program, offered by the Jacobs School of Engineering, that encourages students from all majors to work on projects with non-profit and non-governmental organizations throughout the world.
- The UC San Diego chapter of Engineering World Health, which takes on projects to design, provide and maintain appropriate medical technology for developing nations.
After graduation this spring, Hutchison plans to devote all his time to the new company and push out the viral load test. He doesn’t expect Worldcare to be a big moneymaker. “This isn’t the kind of product that makes a large profit or one that investors throw a lot of money to,” he said. “It’s truly about the millions of people who need viral load test and can’t get them.”
This year Hutchison changed his major from biology to history. That will allow him gain important background about world health, economies and border issues.
Miniscule samples from inside a living cell
Prestigious and prize-winning technology, pioneered by UC Santa Cruz biomolecular engineering professor Nader Pourmand, PhD, has shown great promise for studying and treating cancer and neurodegenerative diseases such as Huntington’s and Alzheimer’s.
Now, his biosensor and nanopipette technology offers the basis for cost-effective diagnostic tests for Zika, Ebola, pandemic influenza and other infectious diseases that plague developing countries.
This summer, Pourmand, leader of the Biosensors and Nano/Bioelectrical Technology Group at the UCSC School of Engineering, won the $300,000 first-place prize in the Follow That Cell Challenge sponsored by the National Institutes of Health (NIH).
He was recognized for technology, developed over 15 years, that allows scientists to take microscopic samples from inside a living cells remarkably, without damaging the cell’s activity or vitality.
“It is the only technology I know of that enables us to interrogate a single cell without killing it,” said Pourmand. “This is a fundamental platform technology with a wide range of potential applications.”
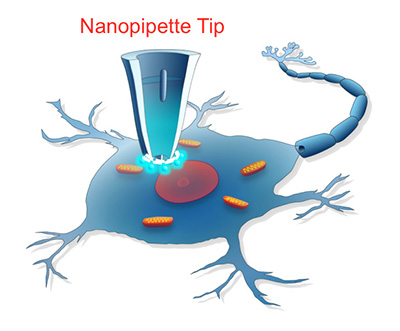
It is a nanopipette platform based on a tiny glass tube that tapers to a fine tip less than 100 nanometers in diameter. That’s a thousand times smaller than the width of a human hair. The nanopipette, which doesn’t disrupt the cell because the tip is so tiny, allows researchers to repeatedly draw samples from the same cell to analyze changes in gene expression that occur in response to therapies.
Pourmand has used the technology to understand how cancer cells become resistant to chemotherapy drugs and to monitor genomic changes in breast cancer cells over time.
Now, he is teaming with researchers to develop bioelectronic diagnostics to recognize viruses, bacteria and fungi that are at the root of some infectious diseases that are endemic in poor countries. With Pourmand’s nanopipette technology as the key player, a general-purpose device would use swappable cartridges to detect specific pathogens in samples of blood or other body fluids. Results could be displayed in seconds on a smartphone app, and uploaded to a cloud-based repository for analysis and integration with existing health networks.
The tests to detect diseases such influenza, Zika and Ebola would be accurate, instant, portable and low-cost — especially suitable in remote regions with limited health facilities and doctors.
Pourmand is collaborating with Pinpoint Science, a San Francisco startup working to commercialize this technology and explore applications that can address current threats to global health.